Reflecting back on the few weeks after Teddy’s first surgery makes me wish we had tried harder to not be so stressed during that time, so we could have conserved our energy for what was to come. Looking back now, those first few weeks were relatively calm. Teddy was stable and his body was doing exactly what the surgeons hoped it would do. Even knowing these things, it was so hard to see our baby sedated and paralyzed. We were not able to hold him and that felt like torture, but in those first few weeks we began to build a routine. It really is strange how quickly a challenging time can just become a normal routine. While our days were anything but normal, even compared to our daily hospital life just a few days before, for us we just settled in and made the best of the situation we were in.
In the NICU we were not able to spend the night. While they couldn’t exactly kick us out, we were not allowed to sleep there, which for me was an extremely hard part. As I have mentioned in the past, being away from Teddy is extremely hard for me. I was and am so scared something is going to happen and I am not able to get to him. While we took turns sleeping in his room while he was on the “floor”, I knew Jason was there on the days I wasn’t there, which made the anxiety better. During these days in the NICU though, this fear continued to grow. I desperately tried not to think about it and put it in one of those silos I am so good at building, but the anxiety found another way to rear its ugly head, which was in the form of a rash on my lower legs. While I had developed this rash while we were in Louisville, it was very minor and only slightly annoying. After Teddy’s first surgery in Boston, however, this rash began to progressively get worse. I will talk more about it later in the story, but I felt it important to share here, because it shows that even though we were staying positive and falling into a routine, the underlying worry was starting to eat away at us.
In the two weeks between surgeries, the days were basically the same. We would wake up at 5:30am to make sure we would make it to the hospital by the time rounds started. I wanted to make sure to always be there to hear exactly what the team was saying about Teddy. This is something we had been doing since Teddy’s birth and the doctors got used to us being there and being part of the discussion when needed. After rounds we would settle into the day. Usually that was getting coffee and ordering or going to get breakfast. We weren’t allowed to eat in the NICU, so we would take turns usually eating in the break room. We pretty much did this for every meal and then sometimes grab dinner at the food court near the hospital on our way back to family housing. I was also pumping, so every 3-4 hours I would go pump. We would help with cares as much as we were allowed to and would sing and read to him. We started going to a parent group, where we would talk to other parents going through the same situation. At the end of the day, they would convince us to leave and go home to sleep. I would typically call at least 2-3 times throughout the night to check on him and then we would wake up by 5:30am the next day and start it all over again.
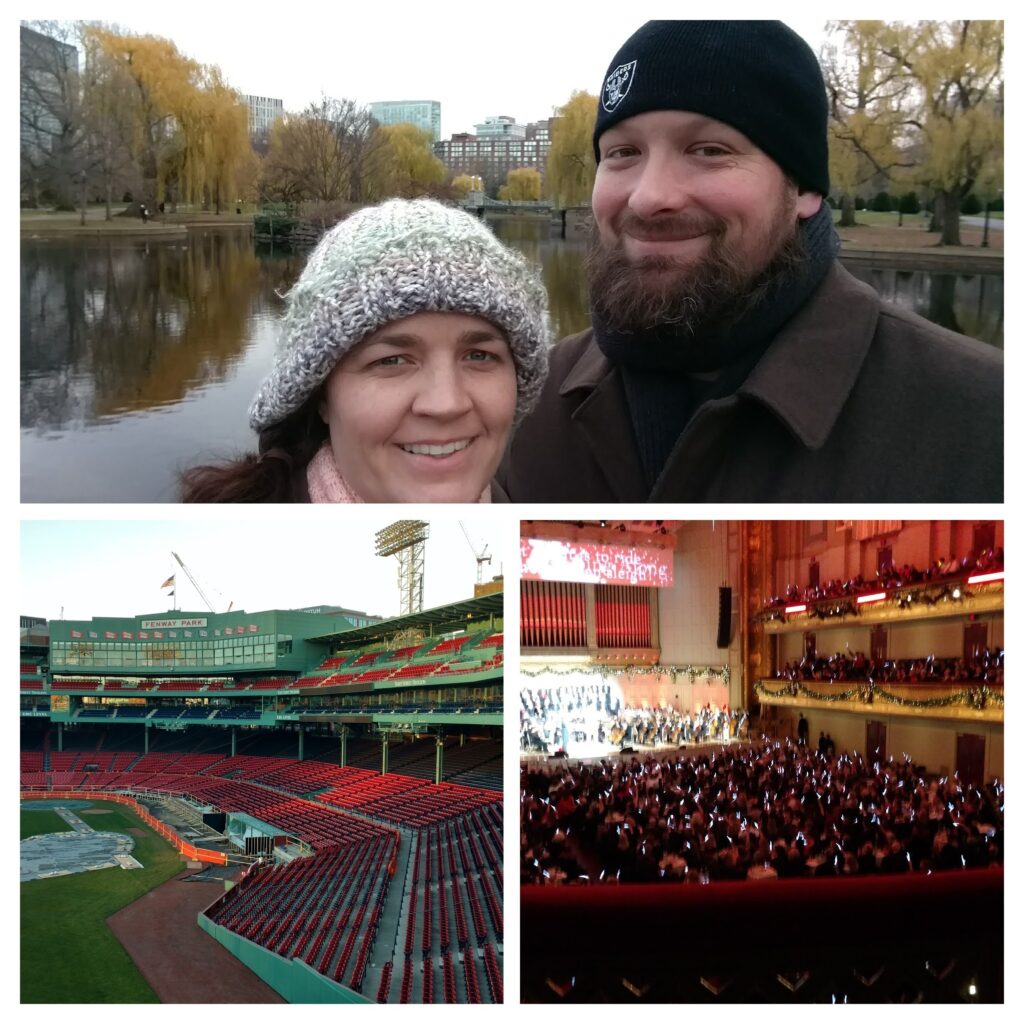
Honestly, I rarely left his bedside and if I did it was for as short a time as I could manage. It became a running joke later in our NICU stay that I was basically a permanent fixture in the NICU, but I truly struggled to breath when I wasn’t by his side. The NICU staff did somehow convince Jason and I to actually leave the hospital to do something other than just go home to sleep, during this time. I am still surprised by this. My mom was staying in the area, so it felt better knowing someone would be there. I had spent 90 days in Boston years before for work, but Jason had never been there, so we did try to see a few things. One day we went to do a tour of Fenway Park. Another day we went to Boston Commons. Family Life for the hospital also had tickets for the Boston Pops Christmas Concert and selected us as one of the families to go. I really didn’t want to go, but it turned out to be so nice and we actually got to sit next to another couple whose son was a micro-preemie in the NICU, and he is a superhero himself. We ended up being “bay buddies” with them a little later in our NICU stay and love getting to know them better and their adorable remarkable son.
Teddy of course was a perfect sleeping angel. He would get agitated a little when being messed with, which you could tell by his vitals, but for the most part he was calm and stable. As far as his routine, it was pretty calm. His cares, feeds, and vitals were all on a schedule. The respiratory therapist would come by a few times a day to check his breathing tube and doctors would come by to check chest tubes and incisions. They did an EEG once or twice to make sure his brain waves were looking good, since he was sedated. Nurses would do wound care and check IVs and PICC/Central lines. It was all very structured and we took that time to get to know Teddy’s nurses and therapists. They were all lovely people and we are so very grateful for them. They all adored Teddy as well and they had yet to even meet him awake yet! His primary day and night nurses were absolutely amazing. They really were responsible for taking care of Teddy and us and did an amazing job. Emily and Molly were truly rockstars and when they did finally get to meet Teddy awake, we were a little concerned they were going to sneak him home with them one day.
Once or twice a day, the surgeons would come by to “stretch” Teddy’s esophagus. I will do my best to explain this process, but you can also look up the Foker Procedure for Esophageal Atresia and get a more technical explanation. There are even a few youtube videos out there that explain all of this better. Since Teddy’s surgery 7 years ago, they have developed an even better Foker procedure and other surgeries that are less invasive and do not require sedation and paralysis while the esophagus is growing like Teddy had to do. Essentially the Foker Procedure uses tension on each end of the esophagus to stimulate esophageal growth. For Teddy, they did this by attaching surgical sutures to each end of the esophagus during the Foker 1 surgery, which they then threaded through the back, so the ends of the threads are exposed. They then tie them off and create a space that they can add “spacers,” that would gently pull the threads each day to put tension on the esophagus to stimulate “natural” growth. I have attached a video and photo below that shows this process, and you can see the little yellow tubes that were used as the spacers.
Every day the surgeons would come in and add a tiny little tube “spacers” on Teddy’s back. I was so surprised when I found these spacers were actually just cut up NG tubes (nasal feeding tubes). You would think it would be some fancy product, but they had found the NG tube to be the perfect size and the easiest thing to use. It only took a few minutes to do and honestly the whole process was pretty simple yet fascinating. After the surgery, the surgeons said it would probably take 2-3 weeks before his esophagus would have stretched enough to do the reconnection surgery, but after about 5 days they felt like it was moving pretty quickly, so decided to move up his esophagram to see how much growth had occurred. Looking back at the photos, I actually laughed because for some reason there were at least 15 people in the room. I really don’t remember why, but I would assume it was because he was intubated and sedated, so they wanted to make sure they could jump into action if something happened, but it was kind of like a clown car in the IR.
But in true Teddy fashion, he completely shocked the surgeons and overachieved in esophagus growth! I think surprising the surgeons by doing the opposite of what they expect is Teddy’s superpower. Sometimes that superpower is a blessing and sometimes it is a curse. Either way, Teddy seemed to have esophagus growing magic happening and really took everyone by surprise. So just seven days after the Foker 1 procedure, Teddy’s esophagus had actually already grown enough for reconnection surgery! This made us very excited, because it meant that he would be awake sooner than we thought and also meant he would not have to be on the medications to sedate and paralyze him for as long as we thought. This would make it easier to wean off of them when the time came.
It would be another three days of waiting before they were able to get him into surgery, but we didn’t mind because it was still one to two weeks sooner than we thought it would be. I will say it was a very long three days of waiting and the closer we got to the surgery, the more nervous I got and the worse my rash got. I was excited this part of the journey would be over, but the fear of the upcoming journey and recovery, which we knew would be the hardest part, made me feel physically sick. After everything he has been through, the surgeries and procedures become routine, but they certainly never get any easier and we knew that this was going to be a big one. So, over those last few days we loved on him as much as we could from his bedside and tried to prepare ourselves for his next major surgery.