We were home again, and it felt amazing. This time my mom had to go back home, so we were completely on our own, but we were so grateful to be home. Don’t get me wrong, it was terrifying and incredibly stressful, but there is just something about being home with your baby, without all the noise and constant interruptions. We absolutely adored our local NICU staff. The doctors were fantastic, and the nurses were amazing. I still think of them as family and know we definitely would not be where we are today without their devotion to Teddy and support of us. With that said, it was so nice to not see them all day every day.
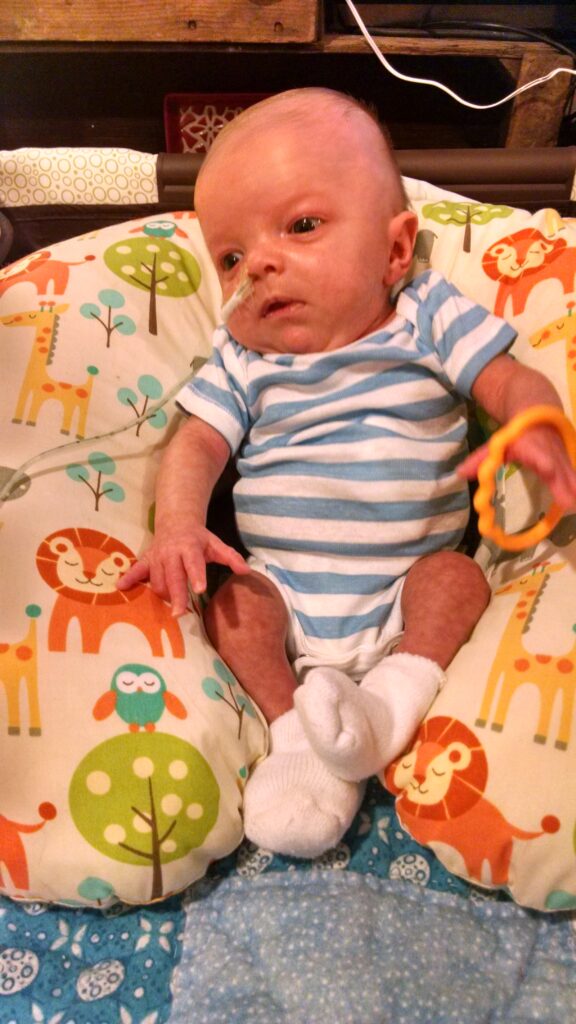
We had our little routine and just took it easy. We found that being in the basement was the best place to spend the day, because we had carpet and more space to have his pack-n-play and various other things including all of his medical equipment. Since he was fed by g-tube, we needed an IV pole to attach his feeding pump too. Ultimately, I would pump breast milk that we would mix with formula to increase the calories. Then we would pour that into a bag that was attached to a pump and a ton of long tubing. The tubing was then connected to a “button” (aka the g-tube) in his stomach, and we would pump the food in over an hour. This was done multiple times throughout the day and night. So, we always had to be close to the IV pole, since it felt like he was connected to his feeding pump, pretty much all day.
Then he had his suction machines and a large battery pack that we used to keep them pulled in while we moved him from one place to the other. One was a continuous suction that was attached to the tube in his nose and on 24/7. It was crucial to suctioning out the secretions (what a fun word) that collected in the top pouch of his esophagus, so that he did not accidentally aspirate (inhale) his secretions into lungs, which would cause him to choke, develop pneumonia, or potentially stop breathing. We also had a secondary suction machine that we used periodically if his continuous suction tube got clogged or overwhelmed and stopped working. We would use it while we fixed the issue causing the issues with the main machine. To ensure his secretions did stay thin, we would also need to give regular saline drops into his nose. We would also change the tube out every couple days, to ensure it stayed nice and clean and open. Can you imagine trying to stick a tube down your nose or throat? Now try to imagine having to do that to an infant. It was horrible, but necessary.
While we were not approved to bring home a big oxygen monitor, we did need to check his oxygen and breathing regularly, so we did that with the Owlet we bought (which is a little sock that the baby wears that has an oxygen probe in it). It wasn’t perfect, but it worked and was much easier to keep on than the larger monitors that we would soon have a lot of experience with. Then add the medicines, syringes, g-tube supplies, suction supplies, etc and you can see our hands and days were full. But we savored every moment!
Teddy was still a great sleeper, so thankfully we were all able to get a little rest. We would play and read and just spend time as a family. We did tummy time, which he HATED, and worked on our PT/OT stretches and activities. One of the days I was laying on the floor in the basement and had him laying on my stomach doing tummy time. He quickly fell asleep, and I just laid there savoring every moment, while I felt peaceful breathing. He truly amazed us every day. We had gone from being told he would not survive to having this beautiful strong little boy at home at only two months old. We knew we had a long road ahead, but he was home.
While we were home, we were finally able to get the second opinion through Boston. They reviewed Teddy’s chart, and the lead surgeon scheduled a call with us to go over everything. This called happened while we were home with Teddy. I can remember the moment perfectly clear. I was on the couch with Teddy sleeping next to me in a bassinet. Jason sat on the steps with Dr. Jennings on speaker phone. The entire conversation was eye opening. First, he was a bit concerned we had taken Teddy home unrepaired (Boston does not allow this), but he also understood that Teddy was stable and why they made the choice to allow us to go home. He told us so much about EA/TEF and everything associated with it and explained why we might be seeing some of the issues with his breathing. He felt that Teddy would be an excellent candidate for the Foker Procedure, but even if testing found he wasn’t, Boston was able to so several other potential surgeries that would repair Teddy sooner. The sense of relief we both felt after that phone call was immeasurable. We immediately decided we wanted to transfer to Boston, and they got the ball rolling. Next, we just needed to try to figure out insurance coverage and how we would get there. We thought we had time though, so we didn’t stress too much.
We had three great days and then on the third day Teddy started struggling to breathe again. His color started turning ashy again and his already fast breathing started to hit the accelerator. So back to the ER we went, again heartbroken and scared. This time he needed high flow oxygen to get his oxygen back up and breathing under control. After several hours in the ER on high flow, they decided we needed to head back into one of the intensive care units. The last time we were able to go back to the NICU, but apparently that was very unusual, since they don’t normally allow patients back after being outside because of the potential germ spread. Because of that this time they sent us to the TICU (Transitional Intensive Care Unit), and it was a complete shock to our perfect little bubble/routine we had created over the last two months. There are very few instances/places in Teddy’s entire medical journey that would say that I would never want to go to again, but I can honestly say that I would never want to be back in that TICU again.
*** For this blog, I have made the decision to not name Teddy’s doctors and nurses (at least not full last names), because I feel like I have the right to share our information, but not the right to share theirs without their permission. The exception to this will be to name Dr. Jennings, because he is so integral to Teddy being where he is today and is world renowned for his work on Esophageal Atresia and a quick google search would identify him anyway (also Teddy went as Dr. Jennings for Halloween one year, so Dr, Jennings is well documented in Teddy’s journey all over my pages).****